CASE OF THE WEEK
2020-9 / MARCH 2
(CONTRIBUTOR: FADI BRIMO)
36 year old male with hematuria was found to have a renal mass, enlarged regional lymph nodes and metastatic lesions in the liver. A biopsy of the renal mass was performed.
Quiz
1. What is the correct diagnosis?
a. Collecting duct carcinoma
b. Renal medullary carcinoma
c. Urothelial carcinoma
d. FH-deficient renal cell carcinoma
1. b
1. Renal medullary carcinoma
Renal medullary carcinoma (RMC) is a rare and aggressive renal tumor typically affecting males of African, Mediterranean, Hispanic or Brazilian descents during their second or third decade of life. Patients commonly present with flank or abdominal pain, hematuria, weight loss and systemic symptoms. Most have metastatic disease at the time of presentation with the lymph nodes being the most common metastatic site followed by the liver, lungs, bone and adrenal glands.
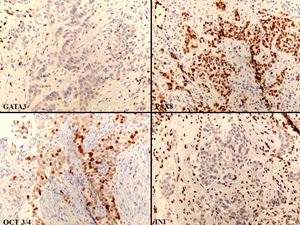
Grossly the tumor is ill-defined and often occupies most of the renal medulla with infiltration of the renal pelvis and hilar/perinephric adipose tissues. Microscopically, the tumor displays many architectural patterns (solid, tubular, papillary, nests, glandular) with the reticular and cribriform pattern being the most characteristic. A desmoplastic stromal response and prominent mixed inflammatory infiltrate are typically present. The cells have eosinophilic cytoplasm, moderate to severe atypia and prominent nucleoli. Mucin production can also be seen. The tumors are positive for pancytokeratins, PAX8, S100A1, and show loss of INI1. OCT3/4 is expressed in about half of cases. Expression of CK7, CK20 is variable.
The characteristic clinical association of this tumor is with sickle cell trait or disease (sickle cell RBCs in this patient are shown in figure 2). Rarely however, tumors with the same morphology and immunophenotype occur in older patients with no hemoglobinopathies, in which case a term such as ‘unclassified RCC with medullary phenotype’ may be appropriate.
RMC has a poor prognosis and most patients are still treated with standard chemotherapy in addition to surgery in selected cases.
Collecting duct carcinoma (CDC) and FH-deficient RCC show overlapping architectural and immunophenotypical features with RMC. As an example, glandular, solid, nested, cord-like patterns of growth are seen in those three entities. Importantly, urothelial carcinoma of the upper tract should first be excluded. Some of the useful diagnostic clues in that differential diagnosis are the following:
CDC affects older patients, usually has a predominantly tubular/tubulopapillary pattern and show retained INI and negative OCT3/4 staining.
Urothelial carcinoma of the renal pelvis also usually affects older patients and show retained INI, negative OCT3/4 staining and is usually negative for PAX-8 and S100A1.
FH-deficient RCC typically has an intracystic papillary and tubulocystic patterns of growth, viral inclusion–like large eosinophilic nucleoli with perinucleolar clearing, is usually INI-positive and OCT3/4- negative. If available, fumarate and 2SC markers are of great utility as the tumor shows loss of fumarate and expression of 2SC.
Ohe C, Smith SC, Sirohi D. Reappraisal of Morphologic Differences Between Renal Medullary Carcinoma, Collecting Duct Carcinoma, and Fumarate Hydratase-deficient Renal Cell Carcinoma.
Am J Surg Pathol. 2018 Mar;42(3):279-292.
Seo AN, Yoon G, Ro JY. Clinicopathologic and Molecular Pathology of Collecting Duct Carcinoma and Related Renal Cell Carcinomas.
Adv Anat Pathol. 2017 Mar;24(2):65-77.
Elliott A, Bruner E. Renal Medullary Carcinoma.
Arch Pathol Lab Med. 2019 Dec;143(12):1556-1561.
Fadi Brimo
McGill University Health Center, Montreal, Canada
fadi.brimo@mcgill.ca
Kidney
Medullary, collecting duct, urothelial, sickle cell