CASE OF THE WEEK
2021-16/ April 19
Contributors: Paulo Athanazio, Daniel Athanazio
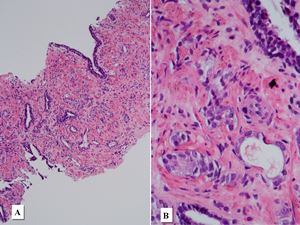
A patient in his 60s underwent prostate needle biopsy due to elevated serum PSA (12 ng/ml) and a PI-RADS 4 lesion at left apex.
(Figure 1 refers to findings in the left base. Figures 2 to 5 refer to findings in left apex.)
Quiz
1. What is the correct diagnosis?
a) Adenocarcinoma + Cryptococcosis
b) Adenocarcinoma + Paracoccidioidomycosis
c) Adenocarcinoma + Malakoplakia
d) Adenocarcinoma + Histoplasmosis
e) Atrophy + Xanthoma
1. c
c. Adenocarcinoma + Malakoplakia
Malakoplakia is a rare histiocytic disease that may occur in any organ. A common site of involvement is the genitourinary tract, particularly the bladder. It is caused by defects in phagocytic or degradative functions of histiocytes in response to gram negative coliforms (E. coli, Klebsiella, Proteus and others) which result in chronic inflammation and intracellular deposits of iron and calcium (Michaelis-Gutmann bodies). It is a well-known mimicker of high-grade prostatic adenocarcinoma. These Michaelis-Gutmann bodies may show overlapping morphology with some fungal species.
In this particular case, Michaelis-Gutmann bodies simulated multiple yeasts with associated buds which were reminiscent of “Mickey Mouse ears” or “boat steering wheel” appearance of Paracoccidioides brasiliensis, a fungus that usually affects patients from South and Central America.
When differential diagnosis of fungal infections and malakoplakia are under consideration, it is important to keep in mind that Michaelis-Gutmann may be stained by Grocott-Gomori’s methenamine silver stain, Periodic Acid-Schiff and Alcian-Blue – the latter a useful tool to highlight the polysaccharide capsule of Cryptococcus sp.
Curiously, some authors believed Michaelis-Gutmann bodies were a particular form of yeast. See reference below (Dickin et al. 1927).
de Souza MF, de Moraes DD, da Costa TP et al. Dealing with prostate cancer? Don’t let histiocytic lesions fool you! Surg Exp Pathol. 2020; 26. https://doi.org/10.1186/s42047-020-00079-8
Dickson WEC, Gray ACE, Kidd F. Malacoplakia vesicae. An investigation of certain mycotic infections of the genitourinary tract. Urol Cutan Rev. 1927; 31,611.
Kwon KY, Colby TV. Rhodococcus equi pneumonia and pulmonary malakoplakia in acquired immunodeficiency syndrome. Pathologic features. Arch Pathol Lab Med. 1994; 118(7):744-8.
McClure J. Malakoplakia. J Pathol. 1983; 140(4):275-330.
Medlicott S, Magi-Galluzzi C, Jimenez RE, Trpkov K. Malakoplakia associated with prostatic adenocarcinoma: Report of 4 cases and literature review. Ann Diagn Pathol. 2016; 22:33-7.
Trpkov K. Benign mimics of prostatic adenocarcinoma. Mod Pathol. 2018; 31(S1):S22-46.
Srigley JR. Benign mimickers of prostatic adenocarcinoma. Mod Pathol. 2004; 17(3):328-48.
Paulo Athanazio
Imagepat, Laboratory of Pathology
Salvador, Bahia, Brazil
Daniel Athanazio
Professor of Medicine, Federal University of Bahia
Imagepat, Laboratory of Pathology
Salvador, Bahia, Brazil
Prostate
Paulo Athanazio
Imagepat, Laboratory of Pathology
Salvador, Bahia, Brazil
Daniel Athanazio
Professor of Medicine, Federal University of Bahia
Imagepat, Laboratory of Pathology
Salvador, Bahia, Brazil