CASE OF THE WEEK
2021-27/ July 6
Contributors: Levent Trabzonlu, Maria M. Pickens, Guliz Akdas Barkan
A male in his 60s with history of prostate cancer status post radiation treatment. Transurethral resection of the prostate is performed.
Quiz
1. What is the correct diagnosis?
a. Papillary renal cell carcinoma, Type-1
b. Mucinous tubular and spindle cell carcinoma
c. Metanephric adenoma
d. Collecting duct carcinoma
e. Clear cell renal cell carcinoma
2. Which of the following is most useful and reliable to distinguish mucinous tubular and spindle cell carcinoma from papillary renal cell carcinoma in a challenging case?
a. CD10 positivity
b. Tumor circumscription
c. Presence of foamy macrophages and papillary structures
d. Low nuclear grade
e. Absence of chromosomal gains in chromosomes 7 and 17
3. Which of the following is associated with adverse histology and aggressive clinical outcome in mucinous tubular and spindle cell carcinoma of the kidney?
a. VST2MA overexpression
b. CDKN2A/B loss
c. Loss of chromosomes 1, 4, and 6
d. CK7 expression
e. PAX8 expression
1. b, 2. e, 3. b
1b. Mucinous Tubular and Spindle Cell Carcinoma; 2e. Absence of chromosomal gains in chromosomes 7 and 17; 3b. CDKN2A/B loss
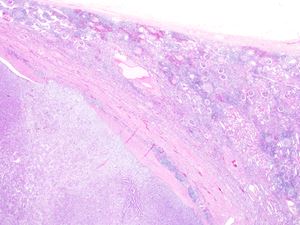
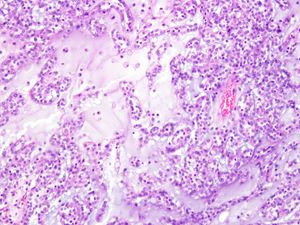
The tumor shows low-grade (ISUP Grade 1-2), tubular morphology with intervening mucinous stroma, and islands of foamy macrophages. Spindle cell component is not prominent. Well-defined papillary structures are not identified. There are no sarcomatous features present. Immunohistochemically, the tumor cells are diffusely positive for CK7 and AMACR; and negative for CD10, CD57, and WT1. The diagnosis was rendered based on the CD10 negativity and the absence of well-defined papillary structures.
Mucinous tubular and spindle cell carcinoma (MTSCC) of the kidney is a rare, low-grade, biphasic tumor first described in 1997 under the name of “low-grade collecting duct carcinoma”.(1) It has a female preponderance with a M:F ratio of 1:3. It can occur in a wide range of age, from 13 to 81 years, with a mean age of 58 years. Most of the cases are found incidentally.(2) MTSCCs may harbor a variety of morphological patterns from the classical morphology with tubular structures, spindle cells, and extracellular mucin to the cases where only epithelioid cords or spindle cells are present in the absence of extracellular mucin.(3) The diagnosis is confirmed by immunohistochemistry and molecular analysis in these cases. Immunohistochemically, MTSCCs are usually positive for CK7, AMACR, and PAX8; and negative for CD10, HMWK, and c-kit.(4) Recently, overexpression of VST2M by RNA ISH has been shown to be sensitive and specific for MTSCC.(5)
The main differential diagnosis is papillary renal cell carcinoma (PRCC) as MTSCCs have significant overlaps with PRCCs both morphologically and immunophenotypically. MTSCCs can show tumor circumscription, tubular and papillary architecture, and foamy macrophages; which are classical morphological features of Type-1 PRCCs. On the other hand, some PRCCs can have predominantly solid growth pattern and sometimes extracellular mucin in rare cases. (6) Both express CK7, AMACR, and PAX8, however, MTSSCs rarely express CD10 while most PRCCs are positive for CD10.(4) Despite the morphologic and immunophenotypic similarities, they are still considered to be two distinct entities as the characteristic patterns of genome-wide copy number alterations of these tumors are different. MTSCCs harbor a variety of chromosomal losses involving chromosomes 1, 4, 6, 8, 9, 13, 14, 15, and 22; while PRCCs show chromosomal gains involving chromosomes 7, 16, 17, and 20.(7) Therefore, distinction between these two entities may require use of ancillary techniques such as VST2M by RNA ISH, FISH or CGH arrays.(8) Other differential diagnoses include metanephric adenoma, other renal cell carcinomas with mucinous changes, and sarcomas or tumors with sarcomatous changes since the spindle component could be prominent in MTSCCs. In most cases, immunohistochemical studies are helpful to distinguish MTSCC from these entities.
MTSCCs are usually of low pathological stage at the time of diagnosis and they have an indolent biological behavior. However, individual cases with sarcomatous features and high nuclear grade have been reported with fatal outcomes in the literature.(9) In addition, CDKN2A/B loss has been reported to be associated with aggressive clinical outcome.(10)
1. MacLennan GT, Farrow GM, Bostwick DG. Low-grade collecting duct carcinoma of the kidney: report of 13 cases of low-grade mucinous tubulocystic renal carcinoma of possible collecting duct origin. Urology 1997;50:679–684.
2. MacLennan GT, Cheng L. Neoplasms of the Kidney. In: Cheng L, MacLennan GT, Bostwick DG, eds. Urologic Surgical Pathology. Elsevier; 2020:83–163.
3. Fine SW, Argani P, DeMarzo AM, et al. Expanding the histologic spectrum of mucinous tubular and spindle cell carcinoma of the kidney. Am. J. Surg. Pathol. 2006;30:1554–1560.
4. Paner GP, Srigley JR, Radhakrishnan A, et al. Immunohistochemical analysis of mucinous tubular and spindle cell carcinoma and papillary renal cell carcinoma of the kidney: significant immunophenotypic overlap warrants diagnostic caution. Am. J. Surg. Pathol. 2006;30:13–19.
5. Wang L, Zhang Y, Chen Y-B, et al. VSTM2A Overexpression Is a Sensitive and Specific Biomarker for Mucinous Tubular and Spindle Cell Carcinoma (MTSCC) of the Kidney. Am. J. Surg. Pathol. 2018;42:1571–1584.
6. Renshaw AA, Zhang H, Corless CL, et al. Solid variants of papillary (chromophil) renal cell carcinoma: clinicopathologic and genetic features. Am. J. Surg. Pathol. 1997;21:1203–1209.
7. Ren Q, Wang L, Al-Ahmadie HA, et al. Distinct Genomic Copy Number Alterations Distinguish Mucinous Tubular and Spindle Cell Carcinoma of the Kidney From Papillary Renal Cell Carcinoma With Overlapping Histologic Features. Am. J. Surg. Pathol. 2018;42:767–777.
8. Trpkov K, Hes O, Williamson SR, et al. New developments in existing WHO entities and evolving molecular concepts: The Genitourinary Pathology Society (GUPS) update on renal neoplasia. Mod. Pathol. 2021. doi:10.1038/s41379-021-00779-w.
9. Dhillon J, Amin MB, Selbs E, et al. Mucinous tubular and spindle cell carcinoma of the kidney with sarcomatoid change. Am. J. Surg. Pathol. 2009;33:44–49.
10. Yang C, Cimera RS, Aryeequaye R, et al. Adverse histology, homozygous loss of CDKN2A/B, and complex genomic alterations in locally advanced/metastatic renal mucinous tubular and spindle cell carcinoma. Mod. Pathol. 2021;34:445–456.
Levent Trabzonlu, Maria M. Picken, Guliz Akdas Barkan
Loyola University Medical Center, Department of Pathology and Laboratory Medicine
Maywood, Illinois, USA
Kidney
Kidney, mucinous tubular and spindle cell carcinoma, papillary renal cell carcinoma